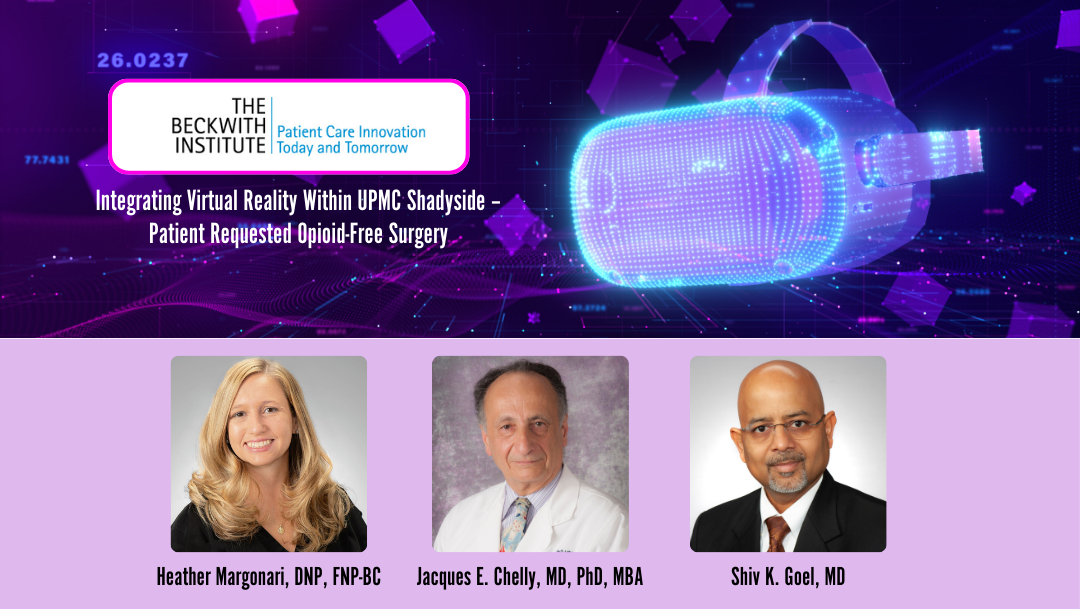
The Beckwith Institute has awarded funding to support a project that will assess the complementary role of virtual reality (VR) in surgery for patients who do not wish to receive opioids at UPMC Shadyside. Spearheaded by principal investigator Heather Margonari, DNP, FNP-BC, the project “Integrating Virtual Reality Within UPMC Shadyside – Patient Requested Opioid-Free Surgery” will be conducted in collaboration with Jacques E. Chelly, MD, PhD, MBA, Director of Acute Pain Clinical Research, Director of our Center for Complementary and Alternative Medicine, and Co-Director of our Center for Innovation in Pain Care, and Shiv K. Goel, MD, Chief Anesthesiologist at UPMC Shadyside Hospital.
The VR project aims to enhance UPMC Shadyside's recently launched Patient-Driven Opioid-Free Surgery (PDOFS) Program. This interdisciplinary initiative includes surgeons, nurses, CRNAs, pharmacists, and hospital operations staff, working together to support opioid-free surgical care. The new project will integrate virtual reality (VR) as an additional non-pharmacological tool for managing pain and anxiety, helping to reduce the need for opioids.
The PDOFS program addresses a growing demand from patients who prefer to avoid opioids during surgery. It is based on regional anesthesia, non-opioid pain relievers, and complementary therapies. The success of the PDOFS is underscored by recent data from a review of 571 patient charts. Among these, 110 patients enrolled in the opioid-free pathway, with 79 patients (72%) completing various elective surgeries using this approach. Only 10 patients chose to withdraw, two received opioids intraoperatively, and 19 required minimal opioids in the post-anesthesia care unit, with no further opioid use during their inpatient stay. This data reflects the effectiveness of the PDOFS in providing safe, opioid-free pain management while maintaining high patient adherence.
The goal of the newly funded VR project is to enable patients to use VR alone or alongside other techniques, such as music therapy, aromatherapy, and relaxation, to help manage perioperative pain. This initiative will focus on selecting appropriate VR content and training staff to establish a pilot program, with a target of full operational implementation by August 2025.
Despite new guidelines reducing the use of opioids, opioid use disorder (OUD) poses substantial risks to surgical patients. It is currently estimated that approximately 1-4% of surgical patients receiving opioids will develop OUD. The UPMC Shadyside PDOFS is already making strides by implementing multimodal perioperative pain management, integrating non-opioid analgesics, regional anesthesia, and complementary therapies such as acupuncture and hypnosis. VR now promises to add a new dimension to this program by enabling patients to manage their pain and anxiety in a personalized, immersive environment.
The project will collect quantitative data on opioid use during hospital stays and associated adverse effects, alongside qualitative data on patient-reported pain levels, anxiety, and overall satisfaction. VR's impact on reducing preoperative anxiety and postoperative pain will be tracked through structured surveys and interviews with patients and healthcare providers.
The data gathered on VR's role in pain perception, psychological outcomes, and patient engagement will inform future clinical practices and protocols, supporting the potential scalability of VR within UPMC and beyond. The initiative will offer a model for other institutions seeking to integrate cutting-edge, opioid-free pain management solutions into surgical care.
This project stands as a crucial step toward a sustainable, opioid-free surgical pathway, with the potential to influence practices across UPMC and contribute to broader efforts to address the opioid epidemic through innovation in pain management.
