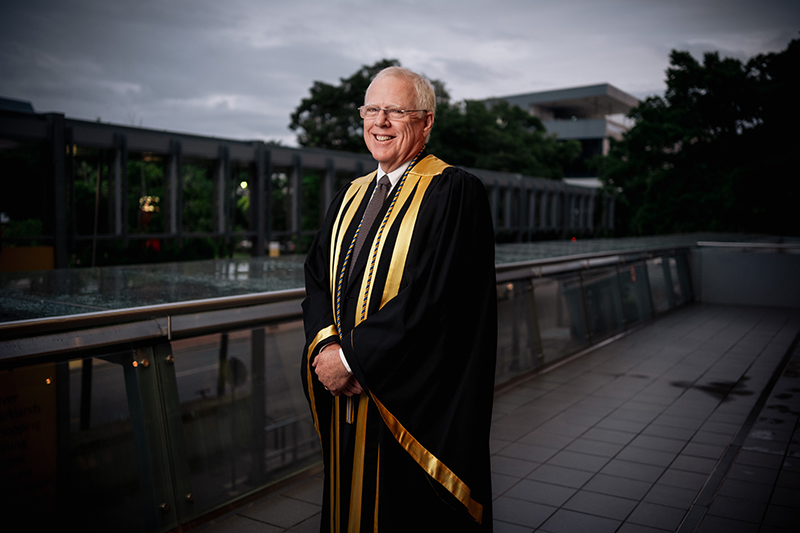
We had the pleasure of catching up with Richard H. Riley, MBBS, FANZCA, D.ABA, FSSH, a distinguished alum of our department. Dr. Riley completed his medical degree at the University of Western Australia (UWA) before coming to Pittsburgh to join our department for his residency training. He also completed a research fellowship with us, graduating in 1985. One fun fact about Dr. Riley is that he played a key role in establishing and managing our alumni group on Facebook, which later evolved into our department's official Facebook page, building our capacity to reach alumni, faculty, trainees, and friends far and wide.
After returning to his native Australia in 1985, Dr. Riley became a trailblazer in anesthesiology and medical simulation, earning recognition as one of the nation’s foremost experts in the field and receiving the Simulation Australia Award in 2011. His impressive career has included leadership roles such as Chief Editor of Australasian Anaesthesia for over a decade and Clinical Director of the Centre for Anaesthesia Skills and Medical Simulation at UWA, where he helped transform simulation-based healthcare education in Western Australia. He also conceived and edited both editions of the Manual of Simulation in Healthcare, a highly regarded text that has shaped simulation-based training worldwide. It received the British Medical Association’s Book Award (First Prize, Basis of Medicine) in 2009.
Among his numerous accolades, Dr. Riley received the ANZCA (Australian and New Zealand College of Anaesthetists) Medal in 2024, recognizing his extraordinary contributions to the field of anesthesiology. He is a past Chair of the Western Australian Simulation in Healthcare Alliance and is currently a Clinical Associate Professor of Anesthesiology at UWA Medical School and Clinical Debriefing Project Manager at the University of Notre Dame Australia School of Medicine.
Dr. Riley spent some time with us to reflect on his journey from completing his anesthesiology training in Pittsburgh to becoming a highly respected leader in medical education and to share insights into his remarkable career, offering words of wisdom for aspiring anesthesiologists.
What motivated you to pursue a career in anesthesiology, and how has the field changed since you first began your training?
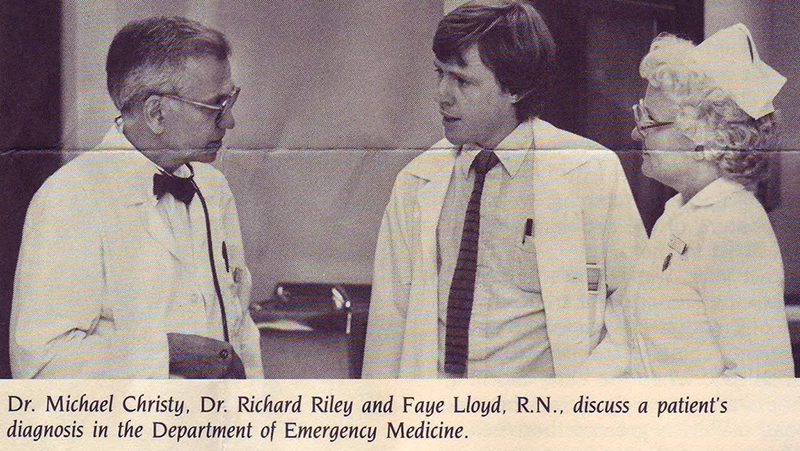
I was always interested in the fields of acute care medicine – critical care medicine (CCM), anesthesiology, and emergency medicine (EM). As EM was not a recognized field in Australia in the early 1980s, following my internship in Perth, I took a gamble to move to Pittsburgh, where Dr. Ronald D. Stewart was setting up the Center for Emergency Medicine of Western Pennsylvania. During that first year, I was lucky to complete a term in anesthesiology, when Dr. Peter Winter was Chair of the University of Pittsburgh Department of Anesthesiology and Critical Care Medicine. I then realized that my future was in anesthesiology. During my training, and immediately after that, I witnessed the introduction of newer devices to enhance patient monitoring (capnography, oximetry) to make our role easier, and almost certainly, safer. Newer drugs with improved safety profiles have also been very welcome.
Reflecting on your time with the University of Pittsburgh/UPMC, what aspects of your residency and fellowship had the greatest impact on your career?
UPMC Anesthesiology placed an emphasis on training and innovation. Grand rounds, for example, were attended by some of the “who’s who” in anesthesiology. There was a “critical mass” of anesthesia experts in the audience. I dared to hope that one day I could join the ranks of senior colleagues, such as Drs. Peter Winter, Miroslav Klain, Peter Safar, Achiel Bleyaert, Ryan Cook, Etsuro Motoyama, Charles Buffington, Yoo Goo Kang, Michael Pinsky, Edwin Nemoto, and many others. I am forever grateful for my mentors, teachers, and the anesthesiology research team at Montefiore Hospital.
Are there any particular memories or mentors from Pittsburgh that stand out as pivotal to your development as an anesthesiologist?
Peter Winter took a gamble by accepting me into the program outside the residency match; I am forever thankful for his generosity. Dr. David Wilks became my mentor and his uncritical guidance and friendship in my early years was pivotal. There were many outstanding teachers and leaders in the fields that I had the privilege of learning from. Professor Miro Klain was inspirational. He was a former cardiothoracic surgeon in Prague and a researcher in artificial organs, who then retrained in anesthesiology and CCM and then developed high-frequency jet ventilation! It was a no-brainer to undertake a research fellowship with his supervision.
How did your experience in Pittsburgh shape your approach to leadership and collaboration in healthcare?
UPMC included a large cohort of leaders. I learned that there was always someone who was very knowledgeable in a neighboring office or just across the road. There was collaboration among researchers from different domains that was encouraging to me. It was rare to see one-upmanship, and it was reassuring to see credit being given to trainees, anesthesia nursing staff, technicians, and others who contributed. The “can-do” attitude was infectious.
What inspired your interest in medical simulation, and how did you envision its potential when you first started working in the field?
Like many anesthesiologists, I was a technology “geek.” I saw an early version of a healthcare simulator developed by David Gaba on a TV program. I wanted one. When it became commercialized, I was fortunate to become involved in its introduction in Perth. Finally, we had a tool to allow anesthesia personnel to train and to rehearse management of all the crises that can occur. It was both exciting and frightening. Now, others could watch me struggle to get out of trouble. I had to learn to be vulnerable if I was to encourage others to participate.
Receiving the ANZCA Medal is a tremendous honor. What does this recognition mean to you, and what would you say has been your most fulfilling contribution to the field?
It was recognition of a long-term commitment to anesthesiology education. It probably helped that I edited our college’s book for 16 years, assessed anesthesiologists trained abroad, accredited simulation centers throughout Australia, New Zealand, and Hong Kong, oversaw the 2.5-day compulsory simulation (“E.M.A.C.”) courses, and accredited anesthesia departments to train anesthesiologists.
As Chair of the Western Australian Simulation in Healthcare Alliance, what initiatives or advancements are you most proud of leading?
Gathering simulation colleagues from all healthcare disciplines together to share research and challenges. Meetings allowed simulationists from universities, hospitals, and ambulance services, including our Royal Flying Doctor Service, to network and share successes.
What advice would you give to young anesthesiologists who aspire to balance clinical practice, leadership, and research in their careers?
If a shy boy from a wheat and sheep farm can contribute in a small way, you can too. I still carry with me two aphorisms from my mentors: “You need to have a gimmick (niche interest),” [Miro Klain]; and “Never accept rejection from a medical journal, keep rewriting” [Michael Pinsky].
What qualities or skills do you believe are most critical for anesthesiologists who aspire to leadership roles in the field?
Start small with publications. Consider a structured course in biostatistics or clinical research after you have finished training and board (college) exams. Most of all, choose a subspecialty that you love.
How has staying connected with the University of Pittsburgh/UPMC alumni community influenced or supported your professional journey over the years?
I continued to visit Pittsburgh most years, as much as my wallet would allow. Combining visits to “the ‘Burgh” to visit lifelong friends with a conference (IMSH or ASA) made it easier. Seeing some of my fellow trainees occupy leadership roles now has filled me with joy. Pittsburgh has a permanent place in my heart. Also, having a very supportive wife has made all the difference!
